Introduction
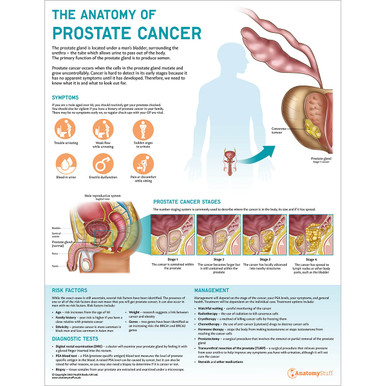
The prostate is the largest accessory gland of the male reproductive system. It secretes an alkaline solution to nourish and protect the sperm as they enter the vagina’s acidic environment. This revision guide will explore the anatomy prostate gland, such as its location, different histological zones and neovascular supply.
Anatomy
The prostate gland is a firm, dense structure weighing approximately 30 grams. It is often described as the size of a walnut, although throughout a male’s life, it can grow significantly in size.
Function
The main function of the prostate is the production of an alkaline fluid. Mixed with sperm cells from the testicles and fluids from other reproductive glands, this makes up the semen. The prostate muscles also ensure that the semen is forcefully pressed into the urethra and then expelled outwards during ejaculation.
Location
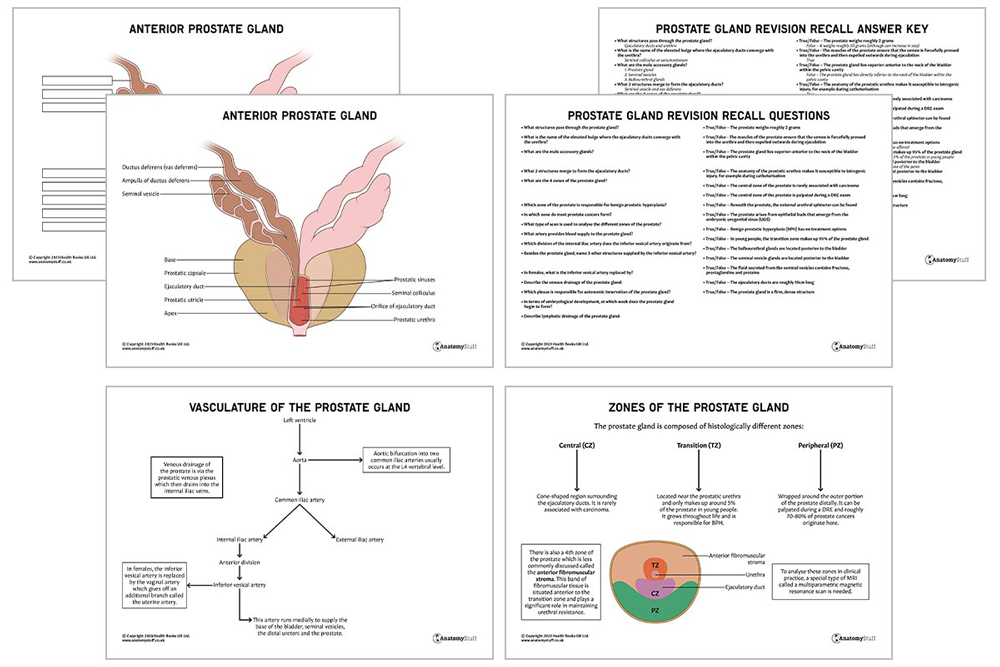
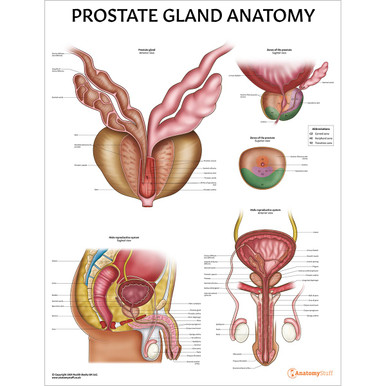
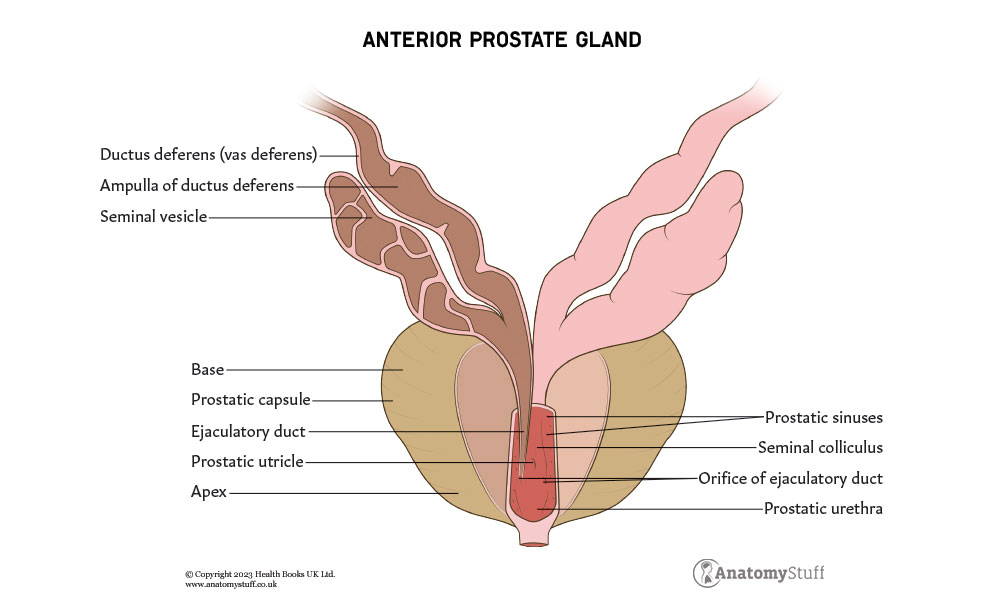
The prostate gland lies directly inferior to the neck of the bladder within the pelvic cavity. The rectum is located posteriorly (making digital rectal examinations (DRE) an easy way for healthcare professionals to palpate the prostate), and the urethra runs almost vertically through the prostate (which is why enlargement of the prostate can subsequently compress the urethra and cause urinary retention).
As well as the urethra, the ejaculatory ducts also pass through the prostate, and they ultimately converge at the urethra at an elevated bulge called the seminal colliculus or verumontanum. Interestingly, in Latin, verumontanum translates to ‘mountain ridge’.
Beneath the prostate, the external urethral sphincter can be found. This structure is composed of striated muscle and wraps around the urethra to help control ejaculatory and urinary flow.
Associated / nearby structures
As described above, various structures are located close to the prostate gland or run through it, such as the urethra and ejaculatory ducts.
Examples of nearby structures include the seminal vesicles and bulbourethral glands. Along with the prostate, these are known as the accessory glands of the male reproductive system, and they all secrete fluids that enter the urethra.
• Seminal vesicle: paired glands posterior to the urinary bladder. The fluid secreted from the seminal vesicles contains fructose, prostaglandins and proteins.
• Bulbourethral glands: paired glands located near the base of the penis. In response to sexual stimulation, the bulbourethral glands secrete an alkaline mucus-like fluid which provides lubrication and neutralises the acidity of the vagina.
On each side of the prostate gland is an ejaculatory duct. These paired ducts are around 2cm in size and are created when the seminal vesicle’s duct merges with the vas deferens. As described above, the seminal vesicles secrete fluid to nourish the sperm, and the vas deferens is a long muscular tube carrying sperm out of the testes. The ejaculatory ducts pass through the prostate and empty into the urethra.
Interesting fact!
It is very important to be aware of the anatomy of the urethra, particularly when performing procedures such as catheterisation. The portion of the urethra that passes through the prostate gland is called the prostatic urethra, and it takes a 30-degree ventral turn toward the bladder when approaching the prostate. This J configuration leaves this portion of the urethra more susceptible to iatrogenic injury, for example, from catheterisation, which can then lead to damage in the form of strictures or bleeding.
Histology
The prostate gland is composed of various tissue types, which can be divided into different zones:
| Zones | Location | Relevance |
| Central zone | Cone-shaped region surrounding the ejaculatory ducts | Rarely associated with carcinoma |
| Peripheral zone | Wrapped around the outer portion of the prostate distally | Palpated during the DRE, and roughly 70-80% of prostate cancers originate here |
| Transition zone | Located near the prostatic urethra and only makes up around 5% of the prostate in young people | Grows throughout life and is responsible for benign prostatic hyperplasia (BPH) |
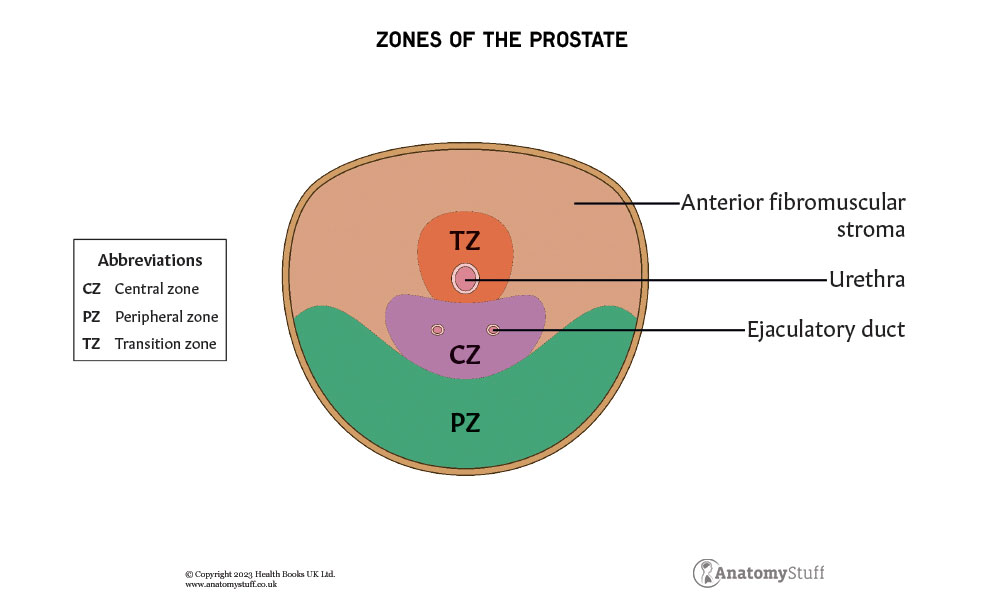
There is also a 4th zone called the anterior fibromuscular stroma. This band of fibromuscular tissue is situated anterior to the transition zone and plays a significant role in maintaining urethral resistance.
A special type of MRI called a multiparametric magnetic resonance scan is needed to analyse these zones in clinical practice. When investigating prostate cancer, the results are reported on a Likert scale and are scored from 1 (very low suspicion of cancer) to 5 (definite cancer).
Blood supply
Due to the close anatomical relationship between the prostate and bladder, their arterial supply is similar. The major blood supply to the prostate is via the inferior vesical artery, which originates from the anterior division of the internal iliac artery. This artery runs medially to supply the base of the bladder, seminal vesicles, distal ureters and the prostate.
The inferior vesical artery branches into two main arterial branches; the urethral, which supplies the transition zone and the capsular artery, which supplies the glandular tissue.
In females, the inferior vesical artery is replaced by the vaginal artery, which gives an additional branch called the uterine artery.
Venous drainage of the prostate is via the prostatic venous plexus, which then drains into the internal iliac veins.
Innervation
The prostate receives autonomic innervation via the inferior hypogastric plexus – (you can learn more about the autonomic nervous system here). Sympathetic innervation is via the hypogastric nerve, and parasympathetic is via the pelvic nerve.
Embryology
The prostate arises from epithelial buds that emerge from the embryonic urogenital sinus (UGS). This begins around week 10 of development.
Lymphatic drainage
The prostate gland primarily drains into the obturator and the internal iliac lymphatic channels. You can learn more about the anatomy of the lymphatic system here.
Surgical relevance
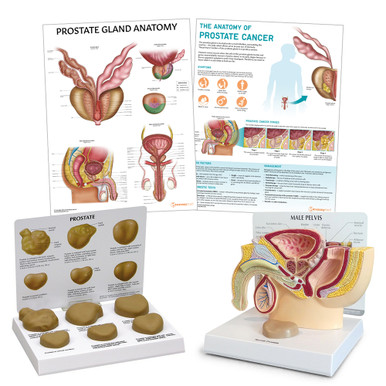
Benign prostatic hyperplasia that has failed to respond to treatment is sometimes managed surgically with a procedure called a transurethral resection of the prostate (TURP). An instrument is inserted through the urethra, and a device is used to shave off different areas of the prostate gland to reduce its size.
Related Products
View All