Understanding Coeliac Disease
Hundreds of thousands of people in the UK have coeliac disease, with a prevalence of one in 100, and out of these, about half a million people are still struggling with unexplained symptoms and do not know coeliac disease in detail. Only about 30% of those affected are diagnosed clinically, and others do not know if they are suffering. The chance of having coeliac disease increases to one in ten if your first-degree family members have the condition.
What is Coeliac Disease?
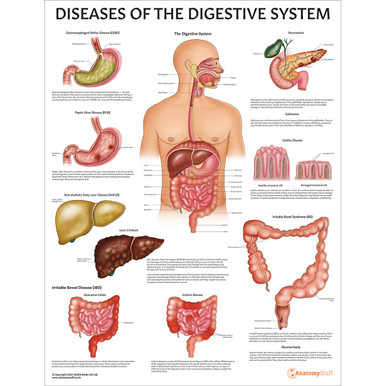
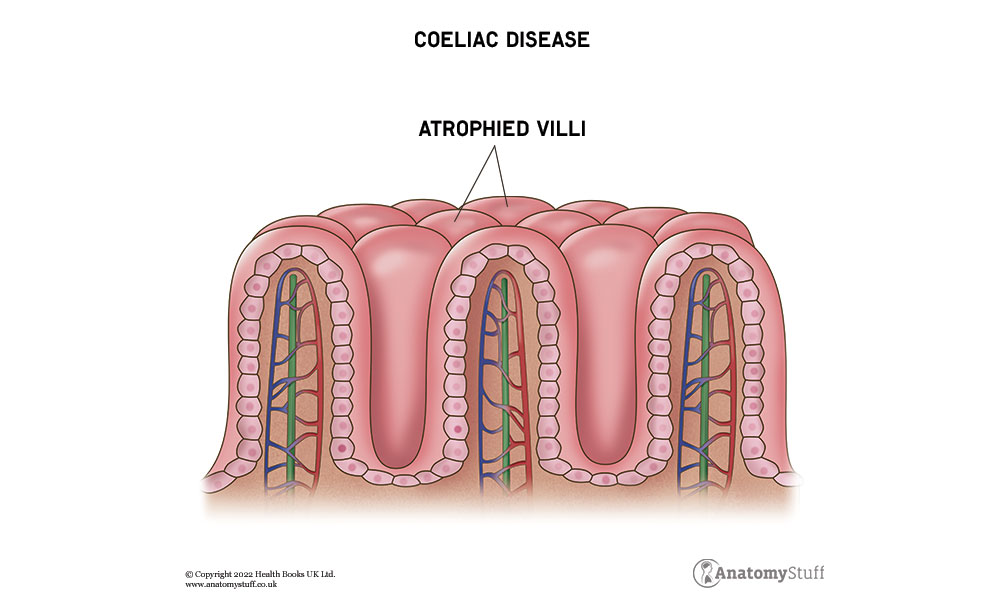
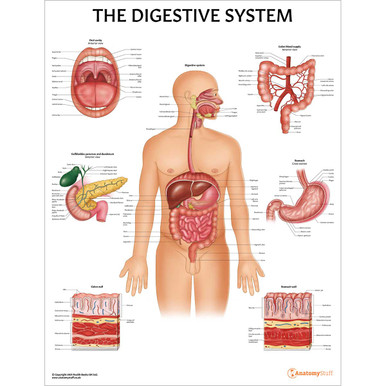
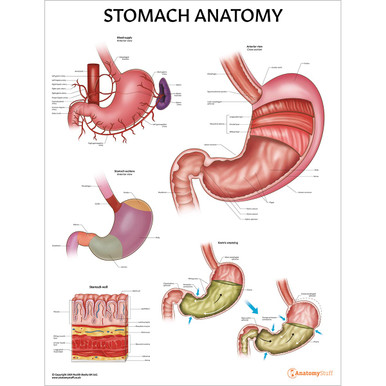
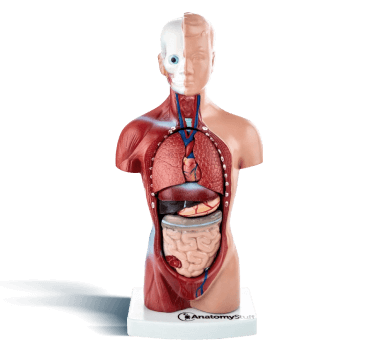
Coeliac Disease, also known as gluten-sensitive enteropathy, is an autoimmune disease characterised by hypersensitivity to gluten (and gliadin), resulting in loss of small bowel villi and malabsorption. Gluten is an alcohol-soluble, water-insoluble protein component of wheat, oat, barley, and rye.
Pathogenesis
It is characterised by T-cell and IgA-mediated response against gluten in genetically susceptible individuals. It is associated with HLA-DQ2 and HLA-DQ8. The highest incidence is in Infancy when a child first starts weaning.
Clinical Features
Coeliac disease is a malabsorption syndrome, which presents with the following clinical features,
• Diarrhoea, weight loss, flatulence.
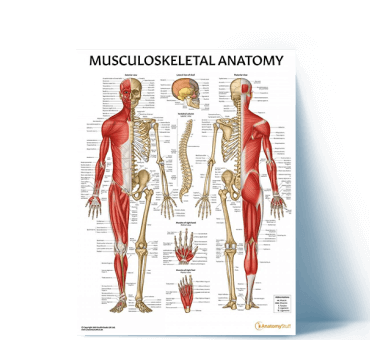
• Malnutrition and osteoporosis.
• Anaemia (Microcytic anaemia – from iron deficiency, and Macrocytic anaemia – from folate deficiency).
• Abdominal pains which tend to come and go, with bloating and diarrhoea.
• Mouth ulcers can be present, similar to those in IBS.
• Weight loss and vitamin deficiencies due to poor absorption of food.
• Dermatitis Herpetiformis (It is seen in 10% of cases, and is characterised by intensely pruritic, papulovesicular lesions on extensor surfaces of elbows, knees, and buttocks.) Immunofluorescence shows IgA deposition at the dermo-epidermal junction.
• In infancy, it presents after weaning onto cereals, with diarrhoea, malabsorption, and failure to thrive. The resultant effects are slow growth, puberty delay, and short stature.
Association
Coeliac disease is associated with other human leukocyte antigen (HLA) — linked autoimmune disorders, such as Insulin-dependent diabetes (type-I), Hashimoto’s thyroiditis, primary biliary cirrhosis, IgA deficiency, Myasthenia gravis, and Non-Hodgkin lymphoma.
Diagnosis
• Endoscopic Biopsy is the Gold-standard test and gives characteristic morphologic features of villous atrophy and blunting. The duodenum and proximal jejunum are the most common sites, with chronic intra-epithelial inflammatory infiltrate (lymphocytic) and crypts hyperplasia.
• Anti-tissue Transglutaminase (tTG) IgA Antibodies: It is an excellent screening test and is more accurate in patients with IgA deficiency.
• Anti-endomysial IgA Antibodies: It is an excellent screening test with a Sensitivity of 85-95% and specificity of 100%.
• Anti-gliadin IgA Antibodies: It is a moderately good screening test, with a sensitivity of 80% and specificity of 85%.
Free PDF Downloads
View AllTreatment
• The mainstay of treatment is a life-long GLUTEN-free diet, which requires omitting wheat, rye, barley, and oats (oats can be started later).
• Correction of deficiencies (Iron, Folate, Calcium, Vitamin D) via supplements.
• Refractory cases may need corticosteroids and other immunosuppressants
• The next best step is Dapsone (100 to 150 mg daily).
What is the difference between Coeliac Disease & Chronic Pancreatitis?
These diseases cause malabsorption, but chronic pancreatitis is not associated with iron or folate deficiency, while coeliac disease is associated with iron and folate deficiency. Normal reabsorption is seen in chronic pancreatitis on the D-xylose test, while there is decreased reabsorption in coeliac disease.
Are there any complications of Coeliac Disease?
Coeliac disease is a malabsorption disease that causes a deficiency of many essential vitamins and nutrients. Moreover, people tend to avoid eating food when they have symptoms of a gluten-containing diet. Diarrhoea and bloating add to the cause, and as a result, coeliac disease causes the following complications in the long term:
• Osteoporosis (thinning of bones due to nutrient deficiency)
• Pregnant women having low birth weight babies and premature births
• Weakened teeth and enamels
• Lymphoma of the gut (a type of cancer)
• Increased risk of developing immune-related diseases such as type 1 diabetes, hypothyroidism, Sjögren’s syndrome, and primary biliary cholangitis.
References
Coeliac disease. (n.d.). Private healthcare | Bupa UK. https://www.bupa.co.uk/health-information/digestive-gut-health/coeliac-disease
About coeliac disease. (n.d.). Coeliac UK. https://www.coeliac.org.uk/information-and-support/coeliac-disease/about-coeliac-disease/?&&type=rfst&set=true#cookie-widget
Coeliac disease | Causes, symptoms, treatment & support | Guts UK. (2021, November 11). Guts UK. https://gutscharity.org.uk/advice-and-information/conditions/coeliac-disease/
Coeliac disease. (2018, November 28). Symptom Checker, Health Information and Medicines Guide | Patient. https://patient.info/digestive-health/coeliac-disease-leaflet
Coeliac UK. (2015, April 20). Eat! Gluten-Free. https://celiac.org/eat-gluten-free/gf-services/coeliac-uk-2/
Related products
View All