What are Pressure Ulcers?
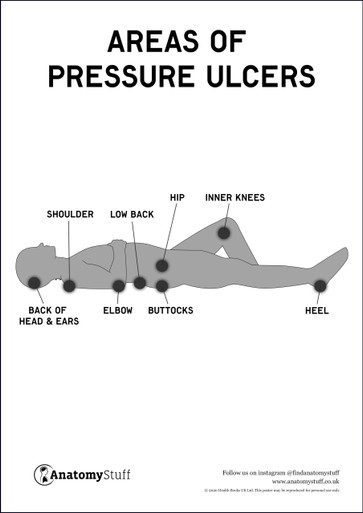
Pressure ulcers (also called pressure sores, decubitus ulcers and bedsores) happen when the skin and underlying tissues are damaged from pressure and blood supply impairment. They typically occur in people who are bedridden, immobile, unconscious, or with neurological conditions. Elderly patients and people with diabetes and circulation problems are at higher risk. Vulnerable pressure ulcer areas include the back of the head and ears, shoulder, elbow, low back, buttocks, hip, heel and the inner knees. Pressure ulcers can develop within hours or days and are usually preventable.
What are the different stages of pressure ulcers?
Stage 1
The skin remains intact but is inflamed, is red or purple and hot to the touch. Symptoms include a burning sensation, pain and itchiness.
Stage 2
The skin is broken, presenting a shallow open ulcer. It may also present with painful blistering.
Stage 3
There is full-thickness tissue loss. The ulcer has a crater-like appearance and has extended to the subcutaneous fat layer. The wound may include undermining (erosion underneath the dermis layer). There is a high risk for infection.
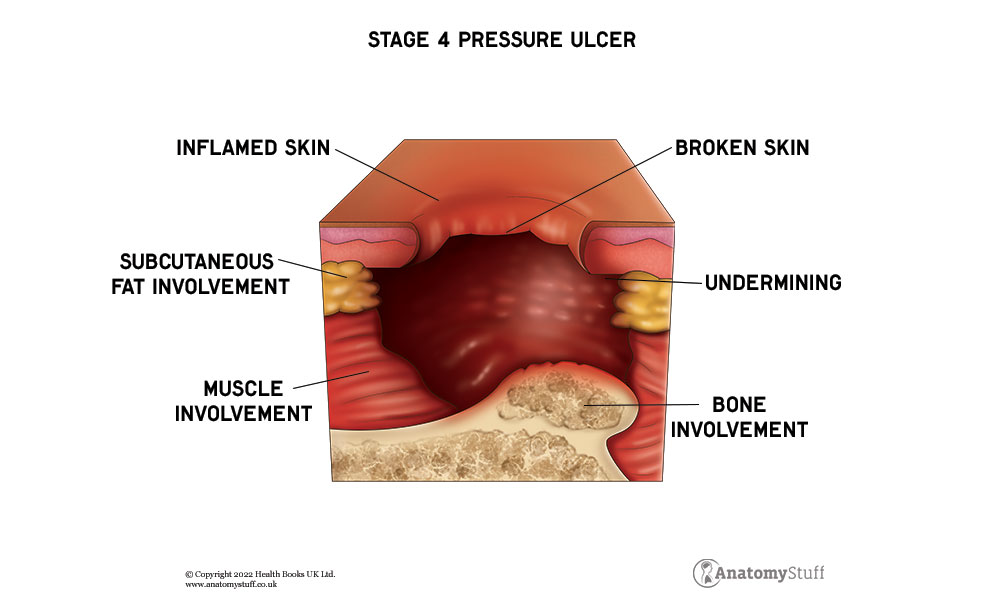
Stage 4
There is full-thickness tissue loss and the ulcer extends to the muscle, tendons or bone. There is often undermining and tunnelling of the skin. The risk for infection and sepsis is now significant.
Prevention of pressure ulcers
• Pressure ulcers may be prevented by regular repositioning of the affected areas. If you are at home, reposition yourself regularly if possible. Patients should be repositioned frequently in line with the care setting policy, to relieve the stress and pressure on the vulnerable areas.
• Look for buttons, any hard surfaces, edges on clothes, wrinkles on bedlinen etc, anything that is crumbled up under the person or anything that can cause pressure.
• Keep the skin dry and clean and use barrier creams as directed. Use barrier creams if the person is incontinent to protect from urine or stool coming into contact with the skin.
• If you smoke, try to quit as smokers are at a higher risk of developing pressure sores, because of the damage caused to their circulation.
• Keep hydrated with lots of water and eat a well-balanced diet high in vitamins, minerals and protein to help keep the skin healthy.
• Regular exercise, where possible is important for general good health and blood circulation.
• Inspect the skin regularly to look for early indicators of skin breakdown, such as redness or discolouration.
Treatment
• Pressure-relieving cushions and mattresses help keep pressure minimised.
• Keeping the skin dry and if required, wound dressings can be applied. If the ulcer needs wound dressings, then a tissue viability specialist or nurse may assess the wound and advice on a dressing plan.
Pressure ulcers, if left untreated, can lead to sepsis (blood poisoning), cellulitis (skin infection) bone or joint infections, initially beginning in the skin and then spreading into the bone. Cancer, a squamous cell carcinoma can even occur from a long-term severe pressure ulcer.