Written by: Zak Shah, 3rd Year Medical Student, UCL.
Maintaining privacy & dignity during invasive procedures
This article has been researched and written by medical professionals for medical professionals alike or anyone with an interest in clinical skills.
A challenging part of working in a healthcare environment is conducting intimate procedures or examinations such as catheterisation or smear tests while keeping the patient relaxed and assured that you respect their privacy and dignity. Though it’s part of the job, and you’ve probably done these procedures more times than you can count, for many patients having procedures in intimate areas may generate a lot of anxiety, especially for patients who are experiencing these procedures for the first time. Equally, while some patients may have had a similar procedure before, the nature of these procedures can still bring about discomfort and the dread of going to see a healthcare provider. For example, a survey by the Department of Health and Social Care in February this year showed that 42% of women who missed their Cervical Smear Tests did not attend due to “embarrassment”.
As clinicians, our job is not only to carry out a procedure or examination but to do so in a way that makes the patient feel reassured, comfortable, and safe. By doing so, we can maintain patient dignity and respect and build a sense of trust in the healthcare profession so that patients don’t feel ashamed to attend important appointments.
Below are some tips to bear in mind to help maintain patient dignity in intimate procedures.
Privacy
Make sure the patient has the procedure (e.g. catheterisation) done in a setting where members of the public will not be able to see or enter. Be wary that not only members of the public should not be able to walk in on the procedure, but other healthcare staff who are not involved in the procedure should not enter the room or setting when it is taking place.
Example scenario:
As you are carrying out an enema on Mr Smith, Jemma, a nurse comes into your hospital room to restock the medicine cabinet.
Although Jemma is a qualified professional, Mr Smith did not consent and was not informed that other healthcare staff would be walking in while he was having this procedure done. This may cause undue discomfort and stress and can result in Mr Smith feeling undignified, with his personal autonomy disrespected.
Instead, you could have a clear do not enter sign to prevent unwanted intrusions and maintain patient privacy.
Explain the procedure
Part of gaining consent is that the consent is informed. Medical terminology can be confusing, especially when patients are already on edge due to sensitive procedures being carried out. To ensure that the consent obtained is informed consent, you should briefly explain what it is that you will be doing to the patient while also explaining the steps you will be taking to maintain their dignity.
Example scenario:
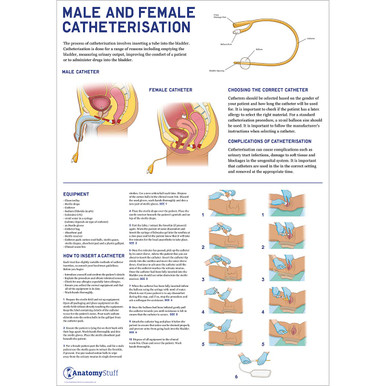
James, 67, is unable to use the bathroom.
Dr Sam says, “Hi, I’m Sam, a doctor. Do you consent to me catheterising you?”
James doesn’t know what catheterising means but is too embarrassed to ask, so consents. During the procedure, he becomes uncomfortable with the idea that something is being inserted into his urethra and feels undignified.
Dr Sam could have made James a more comfortable patient by explaining, “Hi, I’m Sam, a doctor. I will need to insert this catheter into your urethra, which will involve me touching your penis. I will be wearing gloves, and I will also be injecting local anaesthetic, which may sting a little, but will mean the procedure is pain-free. Do you consent to this procedure?”
Above, Dr Sam has taken a minute extra to explain what catheterisation is and made it clear the procedure involves James’ penis. Therefore, James is not taken aback by an uncomfortable surprise and is reassured the procedure will not be painful. Having had the procedure explained to him, James feels more dignified and is happy to go ahead with the procedure.
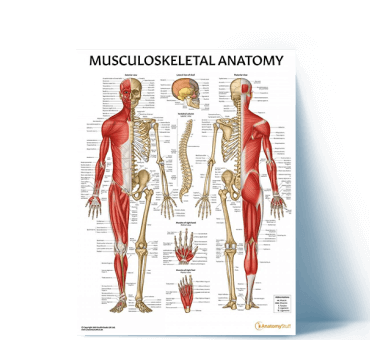
Free Download PDFs
View AllChaperone
Trust Policy may often mandate that a chaperone be present for certain procedures. However, even if a chaperone is not required to be present for certain procedures, ensure that patients are informed of their choice to have a trained chaperone accompany them in the procedure if they wish. This can make patients, particularly vulnerable patients, feel more comfortable when exposing their private parts to you. To help avoid missed appointments, it can be helpful to inform patients of their choice to have a chaperone with them before they have a procedure, for example, by having clear posters and leaflets in waiting rooms.
Example Scenario:
Gillian, aged 28, is scheduled for a cervical smear test. She has reluctantly come to her appointment at the GP but is now having second thoughts while she is waiting, as she doesn’t know what is considered “normal” in these procedures and is worried she may be taken advantage of.
However, she sees a patient information leaflet explaining that a chaperone can accompany her, who is trained to respect her confidentiality and, importantly, knows the standard procedure for a smear test. She is now confident to go into her appointment with a chaperone, and she is better able to trust her doctor.
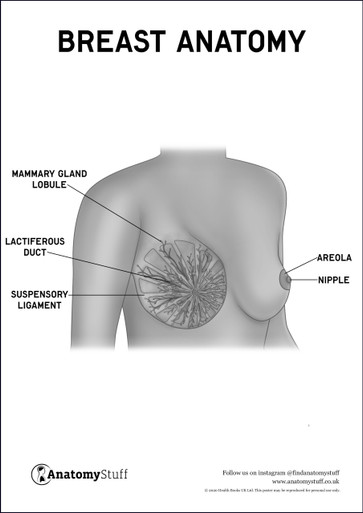
Avoid using less formal words for the patient’s private parts
The patient is placing significant trust in you as a healthcare provider by allowing you to see and touch their private parts in this examination. No matter the personality of the patient, this is a moment when the patient is very vulnerable, and therefore, it is important that you keep to professional boundaries. By keeping to anatomical terminology (e.g., penis, vagina, cervix, rectum etc.) and refraining from other terms that may be commonly or inappropriately used, you firmly establish and reassure the patient that you are acting as a qualified professional and that you are maintaining the professional boundary.
Using commoner words that the patient may use for their private parts should be avoided to maintain the professional boundary and establish that you are a trained professional doing your job with the patient’s safety and wellbeing at heart. At no point should you comment on the appearance of a patient’s private parts unless this is medically relevant.
Example scenario:
Robert, aged 23, requires administration of medication via the rectal route (PR administration). The pharmacist tells Robert that he will be administering the medication via the rectal route. Robert is comfortable that the pharmacist is acting as a professional and feels spoken to in a dignified way.
Related Products
View All