Written by: Zak Shah, 3rd Year Medical Student, UCL.
Medicines Optimisation
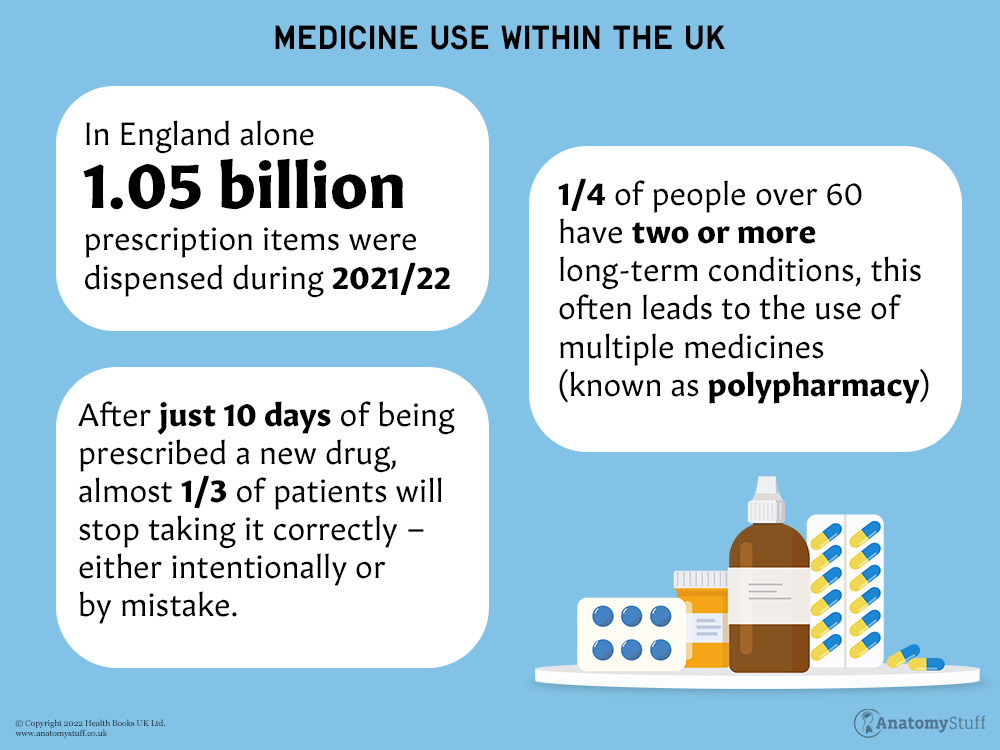
Did you know that after just ten days of being prescribed a new drug, almost a third of patients will stop taking it correctly – either intentionally or by mistake?
And did you know that medication wastage costs the NHS £300 million annually?
Treating a patient doesn’t simply end after diagnosing and prescribing the appropriate drug. What if the patient is on multiple medicines (polypharmacy) that interact, or the patient doesn’t remember which drug to take for which illness?
What if the patient forgets how to take their drug or has unwanted side effects? Perhaps, a new, better medication has come about with greater evidence supporting it.
Medicine Management or Medicines Optimisation refers to the process of making sure patients are prescribed the right drug, are informed about the side effects, and use their medications properly in accordance with the most current guidance for better health outcomes and to reduce wastage and costs.
Medication optimisation primarily involves pharmacists, but doctors and nurses should be involved too – however, most importantly, as stressed by the NICE guidelines, the patient should be involved too in decisions about their drugs.
Involving Patients in their Medications
Medication optimisation often starts with helping the patient choose the right drug for them. The doctor should aim to understand the patient’s experience – for example, asking them if they have had side effects from other drugs before or if they are keeping up with their medication. When patients are faced with several drugs that can be effective, healthcare professionals can use ‘decision aids’ – something like a leaflet that presents information about different medications and treatments to the patient. The patient can evaluate the medications on the decision board, helping them to be informed about their healthcare. This also allows patients to better remember the purpose of their new medication and helps to maintain medication compliance in the future. Prescribers should use an evidence-based approach to prescribing – which means checking that the medicines they prescribe are currently the most effective drugs for the patient.
For patients who are taking several different drugs, which is known as polypharmacy, NICE recommends implementing the approach of “self-management plans”. This allows patients to work out, along with a healthcare professional, a routine that allows them to take their drugs in the best way that works for them and helps them to stay on top of all their different medications.
Pharmacists are your friends!
Pharmacists are the custodians of medication! NICE stresses the importance of communicating with pharmacists, on a regular basis, for medicines optimisation. Pharmacists have a vast amount of knowledge about different drugs, and hence involving them in a patient’s care allows them to check your prescriptions to ensure there are no drugs that are contra-indicated and that the delivery instructions are the most optimum, for example.
Pharmacists should be involved in a patient’s medicines not only from when they are prescribed but also in conducting ‘medicines reconciliation’, which often occurs after a prescription is made, for example, on admission to a hospital.
Medicines reconciliation is the process of asking a patient to list their current medication that they are taking (including any herbal or over-the-counter remedies) and comparing this to the list of medicines that they have been prescribed.
For example:
Roger, aged 74, is admitted for hip replacement surgery. He has been prescribed metformin, ACE inhibitors for his blood pressure, an asthma inhaler, and omeprazole for his stomach for a number of years. However, he has forgotten what omeprazole is used for, so he no longer takes it. He also has been taking a pill that he bought over the counter at the pharmacy that he has not been prescribed. His daughter was given a headache tablet by her GP, which Roger takes from time to time as it helps him feel better.
It is the role of the pharmacist to conduct a medicines reconciliation and find out which of the prescribed drugs (and any non-prescribed drugs) Roger is taking and which drugs he is leaving out. In this example, it is important for the pharmacist to note that Roger is taking drugs that have not been prescribed to him, which may be harmful or dangerous.
The NICE guidelines for medicines optimisation state that “People who are inpatients in an acute setting should have a reconciled list of their medicines within 24 hours of admission”. This is important because the longer the healthcare team is in the dark about patients taking certain drugs that they have not been prescribed, such as in the example above, or patients who are not taking certain medications, the longer the time frame for medication errors, which may be serious, to creep in.
When does medicines optimisation go wrong?
Often, the time when the biggest errors in a patient’s medication occur is when a patient is transferred from one setting to another. This may be a patient being discharged, for example, or may be when a patient changes their care home or is admitted into the hospital. This is because there may be a lack of handover of information, so the patient or carers are not aware of the details surrounding a patient’s medicines. This may lead to patients forgetting their medicines or confusing the dosing regimens.
For medicines to be best effective, it is important that people who are caring for the patient are aware of the patient’s needs and how the medicines should be administered.
This emphasises the importance of having pharmacists involved in various stages of a patient’s transfer, for example, having community pharmacists who are able to assist when patients move to a care home.
When transferring a patient between settings, the following should be documented:
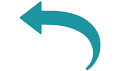
• The date and time of the last dose, for example, if an injection was given last week.
• What information has been passed onto the person and/or their family members/carers
• When medications should be reviewed
• What ongoing monitoring the patient requires if any
• Any support needed to be given to the patient to help them carry on taking their medications.
Although better documentation will improve medicines optimisation, we are all prone to making mistakes which may eventually creep in. Mistakes by healthcare professionals can lead to medicines being administered wrongly, which may be dangerous in some circumstances.
What is to be done when medication mistakes happen?
To ensure that medicine use is as safe as possible, healthcare environments are encouraged to be places that are free of shaming and finger-pointing but instead places where colleagues can learn from one another and admit their mistakes. Healthcare settings should be places where there is what is termed as a “fair-blame culture” – an environment that “encourages the reporting and learning from medicines-related incidents”.
Following Up
With patients who are on multiple different medications, it is important to plan for the longer term too. Medicines optimisation should become much more routine in patient care, and it is important, therefore, to have dedicated pharmacist support. Patients should be followed up with medication reviews (in addition to medication reconciliation). Medication reviews involve a healthcare professional going through the list of drugs a patient is taking and checking that they understand what each drug is for. If a medication was prescribed a while back, the patient may no longer need it but may still, in fact, be taking it. This can be identified and corrected in the medication review. Additionally, patients may have forgotten what a medication does, and this can be explained to them in a medication review.
Healthcare providers should have a long-term view of how they can best practice medicine optimisation and regular feedback to each other about what could be improved.